Medical technologies, more specifically, neurotechnologies cannot progress without the brave women and men who become the early users. Whether they are participants in a first-in-human clinical trial or they are one of the first early adopters, the people who put themselves forward for the advancement of medical technology are Bionic Pioneers. Much like their fellow pioneers in the discovery of flight or space, there are known and unknown risks. Pioneers are those who accept the personal risks for a broader purpose.

There is a rich history of brain implants into humans. We can go all the way back to 1874 when Robert Bartholow demonstrated that electrical stimulation of specific areas of the brain could result in movements. The first-in-human intracranial electrical stimulation, which would then become deep brain stimulation, was experienced in 1952. It would be difficult to gain the perspective of these early brain implant pioneers. In lieu of this, we turn to the early users of modern-day brain implants. The research is amazing, but even more so are the people who are at the forefront of the latest technology.
The early bionic pioneers are mostly people living with paralysis, epilepsy, Parkinson’s disease, amputation, or other neurological conditions. These are the brave souls to take the first step. The list includes names like Cathy Hutchinson, Jan Scheuermann, Ian Burkhart, Nancey Smith, Nathan Copeland, Buz Chmielewski, and Keven Walgamott to name a few. Today, there are over 160,000 people living with a deep brain stimulation and over 35 people implanted with brain-computer interfaces to control movement. Let’s meet some of these early pioneers.
Early First for Humans

Locked-In Syndrome can be caused by a variety of conditions but it tends to be rare in the overall population. It is a taxing syndrome because people living with this condition are cognitively aware, but lack the physical ability to respond. Conversations become one-word answers of ‘yes’ and ‘no. The ability to communicate is a ticket out of jail. Erik Ramsey, had a brain stem stroke at age 16 and is not unable to move any muscle since then. He became a participant in an early study conducted at Emory University and Georgia Tech. Erik became one of the first people to receive an implanted neurotrophic-cone electrode for the restoration of speech. The implanted system is connected to a computer to synthesize speech from thoughts. Expressed by his father, Eddie, the system “gives Erik the hope of being able to break out of the “Locked-In” condition described by Jean Domonique Bauby in “The Diving Bell and the Butterfly.” The system was one of the earliest implanted brain-computer interfaces.
Several years later, another brain interface headline emerged. Being splashed on the news was not what Ian Burkhart was expecting when he became a participant in the Neurobridge study at The Ohio State University (OSU) and Battelle. That is exactly what happened when the announcement from Battelle highlighted the use of brain-machine interface technology to move a paralyzed man’s hand. Ian was that man. A few years prior, Ian became paralyzed while diving into a wave off the North Carolina coast. In a flash, he was paralyzed; losing the two things he treasured, his active lifestyle and his independence. In 2014, we decided to join a clinical trial for a new brain interface. He endured the 4-hour surgery to implant an electrode array into the motor cortex section of his brain. After many sessions in the laboratory, the computer “learned” Ian’s thought patterns and Ian learned how to communicate with the device. This training elevated to thought patterns for specifically moving his hand. The day came when the research team connected the brain system to a functional electrical stimulation sleeve on Ian’s forearm to control his hand. Just by thought, Ian watched his hand open and close. It was pure excitement. Exceeding his expectations, he then drummed his fingers and later played Guitar Hero using the BCI. “There are people out there dedicating their lives to improve ours,” Ian reflects on the research team. “One day (years from now), I will be able to take it home, but for now I will help move the research forward.”
Early Adopters

There are also pioneers who are early adopters of commercial devices. One person that gravitates to the top of the list is Margaret Tuchman who founded The Parkinson’s Alliance. She was, in fact, one of the inspirations of Neurotech Network. I first met her when we were both at the National Institutes of Health campus for a discussion panel. Margaret lived with Parkinson’s disease. When she was diagnosed in the 1980s there was little information available about treatments for PD. She set out to change that through the Alliance and the Parkinson’s Action Network. Nearly two decades after her diagnosis, Ms. Tuchman became one of the first Americans to be implanted with a deep brain stimulation device. She later started DBS4PD.org to help spread information about the device and treatments. While serving on the panel at the NIH, she demonstrated how much it impacted her life. Sitting calmly in a chair on the stage, Margaret turned her DBS off. Almost instantly her severe tremors started and she almost fell to the floor. When she turned the DBS back on, the calmly seated woman returned just as quickly. Until the day she passed away in 2018, Tuchman was a heartfelt advocate and she strongly believed the voice of individuals living with Parkinson’s disease and those who love and care for them must be heard and integrated into the research, policy, and funding process.
Another early adopter of brain interfaces is Mike McKenna who was diagnosed with severe epilepsy. He landed in the ER after driving his van into a canal when he passed out from his first major seizure. From that point forward, Mike’s seizures became more frequent, and they were strong seizures resulting in physical injuries like dislocated joints or broken bones. He was prescribed a slew of medications but nothing seemed to work. Mike found himself jobless, broke, and divorced two years after diagnosis at the Mayo Clinic. His life now revolved around epilepsy. Despite the treatments, Mike was still having grand mal seizures with loss of consciousness and violent muscle contractions. One of his doctors suggested that he participate in a clinical study of the NeuroPace RNS System for refractory focal epilepsy. The RNS neurostimulator is a device that monitors his brain activity 24 hours a day, and recognizes & responds to his unique brain patterns to stop his seizures before they start. It also records Mike’s brain activity, which provides insights that enabled his doctors to optimize his epilepsy care. Mike earned his Bachelor’s and Master’s degrees in social work. He started giving back by working as a Mayo Clinic Social Worker and visiting other people with epilepsy at the Mayo Clinic-Phoenix hospital. He later moved to Portland, Oregon and put his passion to work. Mike is now a Patient Educator for NeuroPace working with others living with epilepsy.
Importance of Options and Preparation
The success stories are always exciting but it’s the failures that also tell the stories. As with any technology, brain interfaces can fail. The recovery from those failures tells the story of resilience as well as the importance of preparations and expectations.
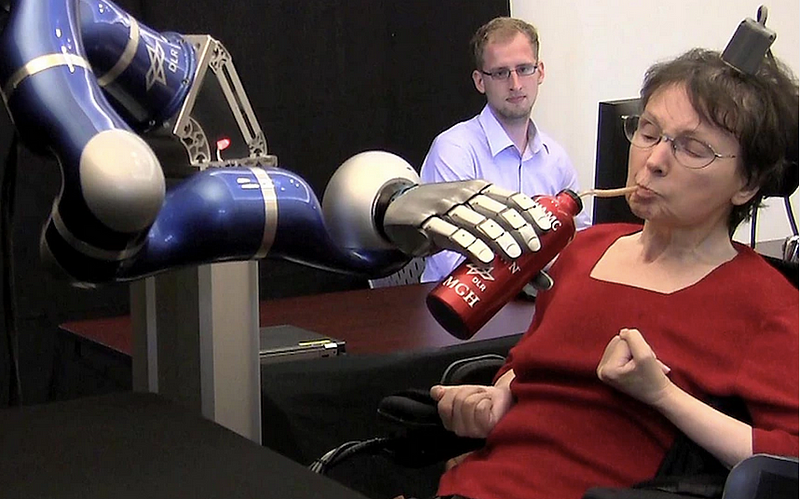
Meet Cathy Hutchinson who had a brain stem stroke at the age of 43, leaving her living with high-level quadriplegia and the inability to speak. In one event, “all my freedom is lost,” she wrote during an interview. Absent of any technology, her communication consisted of eye movements up for ‘yes’ and shaking her head for ‘no’. Without hesitation or fear, Cathy became a participant in the BrainGate project, a consortium between Brown University and Massachusetts General Hospital. Cathy had a small electrode array implanted onto the motor cortex of her brain. When connected to the system, she could adjust environmental controls such as lights, temperature, and music. She could quickly and more naturally communicate with her caregivers, family, and friends. All of this led to her becoming more independent with her daily tasks and opened the door for her to actively interact with the world. Her video and photo were shared around the world when she manipulated a robotic arm to independently drink her beloved cinnamon latte. She did so by using the BrainGate brain interface. Eventually, the signals from her implant started to weaken. In the early use of brain interfaces, this was and still is an issue due to the body’s natural reaction of building scar tissue around the electrode. It came to a point that Cathy could no longer use the brain interface cutting off the communication channel that she once had. She seemed to be prepared for this and accepted the fact that the technology might fail. Working with the research team, they developed an efficient optical gaze communication system for her. Even though she experienced the fluidity of using a BCI, the optical gaze system gave her an alternative tool as she lived out her days.
Jan Scheuermann was also an early BrainGate user but she was working with the team at the University of Pittsburgh. Unlike Cathy, Jan had a degenerative condition called spinal cerebellar degeneration. As she described it, SCD “means that where my brain and spinal cord meet, there is a degeneration of unknown cause.” She was 36 years old when the symptoms surfaced and within a few years she was paralyzed from the neck down. Jan discovered the research team when a girlfriend saw a story about the technology and showed the video to her. Jan thought, “I wish I could do that.” She contacted the research team and became a participant in the BrainGate trial. Her story was featured during a 60-minutes episode titled “Breakthrough: Robotic Limbs Moved by the Mind.” In the video, she demonstrates using her brain interface to manipulate a robotic arm to feed herself a piece of chocolate. When she thought about the future of brain interfaces, Jan wanted the ability to put the device on in the morning, go through a checklist, and then use it all day independently. She imagined that she could use it to brush her teeth, call an elevator or communicate for safety. Jan’s BCI was explanted due to a possible infection. In a conversation only one week following her explant, Jan said that she was comfortable getting the device explanted and she fully understood the risks even before she was implanted. She still experienced the inevitable emotions of missing it. She would miss the technology, the ability, and also the purpose in life as a trial participant. When Jan was first implanted, she welcomed the opportunity and the new purpose in life. When she was explanted, she viewed it as closing a chapter of her life and felt confident that she had the optimism to move forward and the ability to love and be loved for her next chapter.
Whether it is alternative options, mental preparation or conditioning expectations, the technology failures are some of our greatest learning opportunities.
Smart Evolution
As brain interfaces evolve, they should evolve with the end-user in mind. Understanding the preferences, use cases, and unmet needs of the potential end-user drives the intelligent design of the technology. As Margaret Tuchman would advocate, embedding the voice of the person living with the condition is vitally important. There have been a few studies published about preferences more so for brain-computer/machine interfaces for paralysis. One study by Huggins surveyed 61 people living with ALS about their perspectives for BCI and 84% of the respondents stated that they would accept an electrode cap for recording brain signals. However, the desired features had high requirements including a 90% accuracy rate, simple setup, standby reliability, and a variety of available functions.
In another study led by Collinger, they asked 57 veterans living with paralysis due to spinal cord injury about preference and attitudes toward BCI. In this study, the majority of respondents reported the most useful application of BCI would be to control a functional electrical stimulation device to restore movement. Plus, more than 30% of respondents would consider it “very helpful” to use a BCI to control computers and a wheelchair. They also overwhelmingly wanted to use the device independently and placed a high priority for a non-invasive device but would consider a surgically implanted device.
One other preference study led by Blabe, addressed people living with high levels of paralysis and included non-invasive EEG, minimally invasive ECoG, and surgically implanted intracortical electrodes. Their survey included 285 respondents. The top priority of use was to restore upper extremity function. Preferences were for non-invasive devices and there were related concerns of aesthetic factors, daily maintenance, and potential technician interventions. Finally, in a top ten “wish list” published by Hochberg and Anderson, safety, affordability, and reliability took the topic spots for preferences.
These are only a few studies but more needs to be done. The development and evolution of integrated brain interfaces cannot happen in a laboratory vacuum. As the technology evolves so do the use cases and preferences of the potential users. User-centered design is critical for consumer adoption and satisfaction.
Most of the stories within this feature are from people who are the early pioneers of implanted brain interfaces. Surgically implanted devices bring a level of complexity to the decision-making process for adoption and use. What we are missing from these stories are those of non-invasive device pioneers. If you have a story suggestion, please send a message to Neurotech Network to share.
